The right lung has 3 lobes: Right upper lobe, middle and lower lobe.
The left lung has 2 lobes: Left upper lobe (the lingula anatomically corresponds to the middle lobe on the right) and lower lobe.
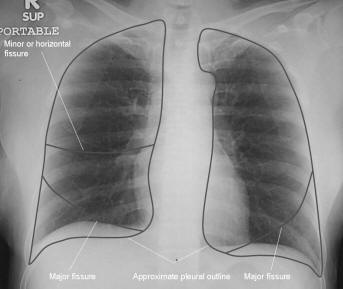
Lobes are separated by fissures - the right major fissure separates the right upper and middle lobes from the right lower lobe. The right minor (horizontal) fissure separates the right upper lobe from the right middle lobe. The left major fissure separates the left upper lobe and lower lobe. Segmental anatomy has little relevance in plain chest radiography.
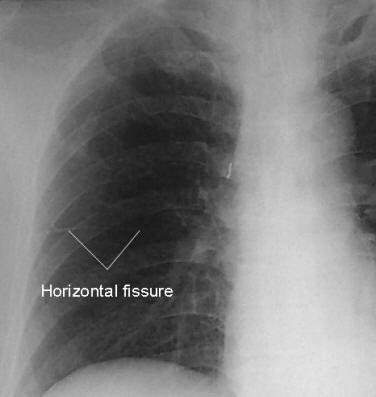
The position of the various lobes on the frontal CXR is illustrated below.
The figures illustrate the CXR appearance of consolidation of different lobes. Because of the loss of the solid-gas interface the heart borders or diaphragms may be obscured by consolidation of adjacent lobes
Right upper, middle and lower lobe consolidation (from left to right)
Left upper lobe,lingula and left lower lobe consolidation (from left to right)
Pulmonary infiltrates
An infiltrate is the filling of airspaces with fluid (pulmonary oedema), inflammatory exudates (white cells or pus, protein and immunological substances), or cells (malignant cells, red cells or haemorrhage) that fill a region of lung and increase the visual impression of increased soft tissue density.
Atelectasis/collapse
Atelectasis is the collapse of the airspaces which also results in the visual impression of increased soft tissue density. This makes it impossible to distinguish infiltrates from atelectasis on the basis of visual density alone. Considering other factors is therefore required. Atelectasis must have volume loss by definition (collapse of airspaces must reduce lung volume), whereas infiltrate does not.
Atelectasis in ICU patients occurs most frequently in the left lower lobe, probably because the heart in the supine position compresses the lower lobe bronchus. The following signs of atelectasis can be seen:
- Mild atelectasis – usually not clinically important
- Basilar shadowing or linear streaks called subsegmental or “discoid” atelectasis
- Severe atelectasis
- Opacification of all or a whole lobe or several segments of a lobe,
associated with volume loss:
- crowding of vessels
- crowding of ribs
- shift of structures such as interlobar fissures or the hilum towards areas of lung volume loss
- elevation of the hemidiaphragm
- Compensatory hyperinflation of adjoining lung may occur.
- Opacification of all or a whole lobe or several segments of a lobe,
associated with volume loss:
Major differentiating factors between atelectasis and pneumonia:
| Atelectasis/collapse | Consolidation |
| Loss of lung volume
Anatomy shifts towards atelectasis Linear, smooth, wedge-shaped Apex of opacity starts at hilum
|
Normal lung volume
No anatomical shift Consolidation
|
| Air bronchograms can occur in both. | |
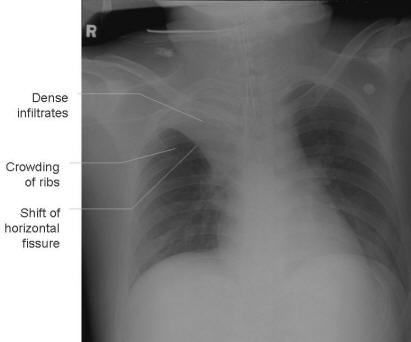
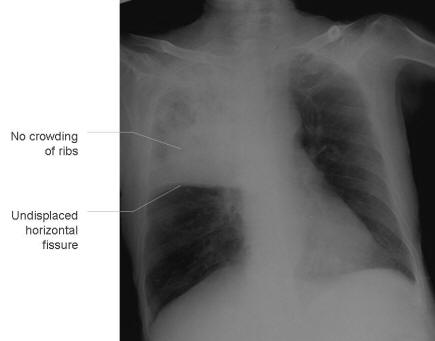
Right upper lobe collapse (left) and consolidation (right)
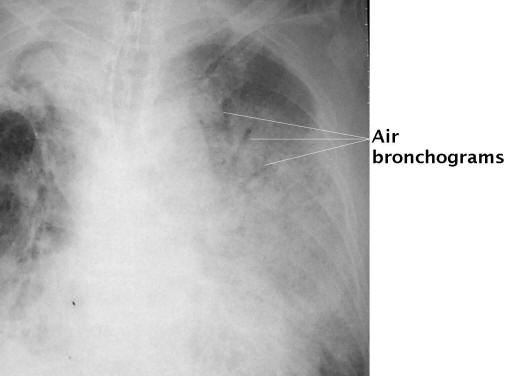
Pneumonia
- Severe pneumonia is classically manifested by airspace disease and consolidation (alveoli and bronchioles that are completely filled with bacteria or other microorganisms, white cells and inflammatory debris)
- Air bronchograms may occur (air in larger bronchi, outlined by consolidated surrounding parenchyma)
- Other
radiographic features include:
- interstitial infiltrates that may be the only manifestation or may coexist with consolidative changes.
- ± associated parapneumonic effusion
- Radioopaque masses, such as tumours can be difficult to distinguish from patches of consolidation, but are generally more well-defined.
- In aspiration pneumonia the lobes affected are dependent of the
gravitational flow of aspirated contents:
- erect patients: right lower lobe
- supine patients: posterior segment of upper lobe and superior segment of lower lobe
- Upper lobe pathology should always lead to the consideration of tuberculosis (TB) as a possibility.
- Pneumonia may be complicated by cavitation or destruction of the lung tissue, creating abscesses.
Acute Respiratory Distress Syndrome (ARDS)
ARDS is an acute response to systemic inflammation. It is difficult to distinguish from cardiogenic pulmonary oedema or pneumonia. While cardiogenic pulmonary edema typically begins centrally in the bilateral perihilar areas, ARDS usually causes more uniform opacification. Pleural effusions are not typical of ARDS but often present in CHF. Kerley B lines are common in CHF but not in ARDS, while air bronchograms can be found in both. The distinction from pneumonia is on the basis of non-radiological investigations.
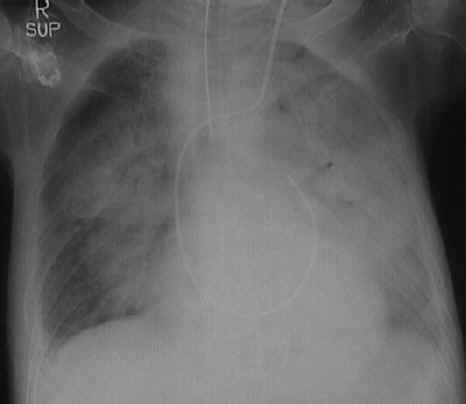
Acute respiratory distress syndrome. The patient is intubated and has a pulmonary artery catheter in situ
Pulmonary oedema
Pulmonary oedema is transudate fluid collecting in the lung tissue. Three
mechanisms lead to pulmonary edema. These are:
1. Increased hydrostatic gradient
2. Diminished oncotic pressure
3. Increased capillary permeability due to endothelial injury
Any one or more often a combination of these mechanisms will cause fluid to enter the alveolar space.
When the capacity of the the lymphatic system is overwhelmed, interstitial oedema results. The classic Kerley lines are made by the thickening of the interlobular septa that carry the lymphatics (Kerley B lines are short thin lines, 1.5 to 2cm in length, seen in the periphery of the lower lung, extending to the pleura). As fluid continues to accumulate, it leaks into the pleural space resulting in pleural effusions and into the alveolar spaces causing the classic alveolar pattern of pareynchymal pulmonary edema.
Congestive heart failure is the most common cause of acute pulmonary oedema, and has additional features to the above because of the mechanism of causation that is primarily the increased hydrostatic gradient. It is often associated with cardiomegaly – difficult to determine on an AP film. Better indications are that the upper lobe blood vessels become more prominent due to vascular congestion (upper lobe blood diversion). The interstitial edema that results from transudation of fluid also affects the interstitium around the vessels and causes an apparent increase in diameter, causing an elevated arteriole to bronchiole ratio. Transudation fluid may also outline the bronchi that run with the vessels, causing peribronchial cuffing.
Note causes of non-cardiogenic pulmonary oedema include aspiration, transfusion reaction, neurogenic, ARDS, renal or hepatic disorders, inhalation of toxins, allergic alveolitis.
Note: A hallmark of pulmonary oedema is it’s ability to clear rapidly – within hours. This may help to distinguish it from pneumonia, ARDS or haemorrhage.
Pulmonary haemorrhage
Presents radiographically like any other alveolar infiltrate (pneumonia, edema). Pulmonary hemorrhage is often resolves more quickly than other alveolar densities such as pneumonia, but not as quickly as improving pulmonary oedema.
Text © Gavin Joynt, June 2005; images © Charles Gomersall, June 2005